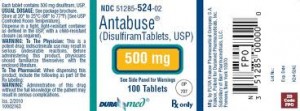
 I want to offer a disclaimer: My opinion of disulfiram, or Antabuse, isn’t based on a review of the research. It’s based on observation and experience (that notorious enemy of convincing-sounding research). At one time, our psychiatrists prescribed it to some 70% of our alcoholic patients post-detox, so I had a chance to watch and take note of the outcome.
I want to offer a disclaimer: My opinion of disulfiram, or Antabuse, isn’t based on a review of the research. It’s based on observation and experience (that notorious enemy of convincing-sounding research). At one time, our psychiatrists prescribed it to some 70% of our alcoholic patients post-detox, so I had a chance to watch and take note of the outcome.
For those who are unfamiliar with Antabuse, it makes you sick when you drink. A few minutes after intake of alcohol, a range of symptoms can appear, commonly including shortness of breath, flushing of the skin, accelerated heart rate, a terrific headache, nausea and vomiting, mental confusion, and in some cases even a brief loss of consciousness. Scary, huh? Most patients find it so. It’s designed to prevent drinking on impulse, but if I’m an alcoholic with a history of impulsive drinking, do I really want to mess with this? What if I screw up –as I have so many times before? Call an ambulance?
This wariness leads patients to come up with some ingenious reasons to go off the medication. Like Margaret, who claimed she couldn’t get the child-proof cap off the refill bottle. Seriously. Said with a straight face.
Doctors sometimes refer to this as a ‘compliance issue’. As in, patients don’t take the med as prescribed, so their blood level remains subtherapeutic, so when they do slip, no aversive reaction, thus defeating the purpose of taking it. Or as one colleague put it: “alcoholic 1, medication 0.”
I did meet a physician who used Antabuse to control his own consumption. He’d experimented on himself to determine the precise point at which the adverse reaction began, and would stop as soon as he felt the initial symptoms. In his view, this was a perfectly reasonable way to avoid overdrinking. Never occurred to him that only an alcoholic would consider such measures.
Some docs have suggested recruiting family members to monitor the patient as he takes his daily dose. I’m sure that works sometimes. I can also imagine a scenario where the alcoholic gets royally fed up with the monitor.
I did ask one doc why he kept prescribing Antabuse when the results were so underwhelming. “It makes me feel that at least I’m doing something for these people,” he replied. I guess you could say the psychiatrist benefited from the medication, even if the patient didn’t.
This is what happens with many medications used to prolong or maintain sobriety. Some patients will swear by them. Others offer tepid endorsement. Still others will find it useless, and a few, like the young physician in my example, will actually incorporate the med into the addictive process.
If an alcoholic is motivated enough to stick with Antabuse, it’s entirely possible he might have succeeded without it. It’s the less motivated for whom we need to find more successful treatments.

 — January 6, 2014 @
— January 6, 2014 @ 






