 What is it about the last dose of methadone or Suboxone that sinks so many well-intentioned attempts to successfully taper off opioid maintenance? I just spent a long lunch listening to a puzzled therapist describe the experience of a longtime patient, and his deep disappointment at the outcome.
What is it about the last dose of methadone or Suboxone that sinks so many well-intentioned attempts to successfully taper off opioid maintenance? I just spent a long lunch listening to a puzzled therapist describe the experience of a longtime patient, and his deep disappointment at the outcome.
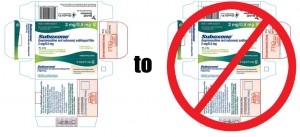
The patient had been on Suboxone OMT from a private psychiatrist for three years. He’d done extremely well, substantially better than his peers. The taper– which had been the patient’s goal from the outset– occurred over the course of a year, and featured careful monitoring and slow decreases in dosage. The patient was actively involved in peer support. The therapist couldn’t have been more pleased with his progress. “And then as we approached the end, right at the end in fact, it went downhill fast. Craving, sure, but much more. All these symptoms hitting at the same time.”
Within a month, the patient was back on the streets, bingeing, risking OD and disease, committing crimes– as if, the therapist reported, the years in between had never happened.
This is a familiar tale. Reliable stats on relapse can be hard to come by, but return-to-heroin rates appear to run above 80% (and in some cases, higher). It’s something that’s long been observed among methadone patients, and seems to be holding for buprenorphine as well.
There are conflicting explanations, falling into two broad groups. The addicts I’ve interviewed describe it in terms of a sudden, dramatic recurrence of withdrawal. For them, it’s perceived as physiological in nature, rooted in brain and body chemistry. As one recovering nurse who’d been through the process reported, “It instantly erases all motivation for staying clean.”
Ironically, the clinicians I’ve talked with see it as psychological— a panic attack or phobic reaction to the loss of the ‘security blanket’ provided by the medication. “It’s just anxiety,” insisted one. “The client could cope, but they’ve built it up in their minds to the point where relapse is a self-fulfilling prophecy.”
“There are all these myths about how awful withdrawal is, that reinforce it,” he insisted. “They’re coming off these very small doses and still getting ‘dope sick’? It makes no sense.”
Well, it makes sense to the addict, which is the important thing. “I don’t encourage a client who’s doing moderately well to try tapering off,” admitted a veteran counselor. But suppose the client wants to taper? “I won’t prevent it. But I certainly don’t hold out much hope.”
I still don’t have a clear picture of the culprit behind the ‘last dose’ phenomenon. If it’s physiological in origin, we should have a coherent theory based in neuroscience. We’d expect as much for any brain disorder. On the other hand, if it’s psychological, shouldn’t we have an evidence-based protocol for treatment — the way we do for, say, chronic insomnia?
Perhaps we’ve tried but failed to come up with such a protocol. There’s some question about the effectiveness of therapy with opioid maintenance clients. Here’s a summary of one NIDA-funded study on CBT plus medication.
There’s the common criticism that OMT programs benefit financially from keeping stable patients on maintenance. Be that as it may, if the vast majority of motivated patients would fail anyway, does it really make much difference?
I wonder if the core dynamic of addiction isn’t more about the relationship between the individual and the drug than about that individual’s psychological health or ability to cope. If so, that suggests that recovery on opioid maintenance is qualitatively different from recovery without it.
Makes sense, doesn’t it? That life on a high dose of opioid would be different from life without it?
I’m not suggesting one is superior, just that they may in fact not be the same.










