 I was talking with a colleague who recently left her job with a methadone maintenance program in another state. Like many ex-staffers, she had mixed feelings about the experience.
I was talking with a colleague who recently left her job with a methadone maintenance program in another state. Like many ex-staffers, she had mixed feelings about the experience.
She was convinced the program provided a valuable service to the community simply by getting people away from a pattern of daily IV heroin use. “I’m sure our clients were better off with us than on the street hustling for heroin.” Many of them were still using, she admitted, but perhaps less frequently, and in less risky circumstances– a clear benefit to public health.
There were things she didn’t like, as well. “Let’s face it, we were a classic client mill. Caseloads were always full, counselors were overworked and underpaid, morale was low, turnover was high. At one point we had over 800 people on our rolls, and it was all we could do to just keep up.” It wasn’t like treatment in other programs, she explained; it was more along the lines of check-in visits with a probation officer.
For her, the biggest challenge was the lack of support for the notion that maintenance clients could someday taper off methadone. It was frankly discouraged. The program’s goal was to stabilize the client on meds and then keep her there as long as possible. The rationale: An elevated risk of return to heroin. “I’m sure that’s true,” she acknowledged, “but I know a self-fulfilling prophecy when I see one. We weren’t trying, so our clients didn’t, either.”
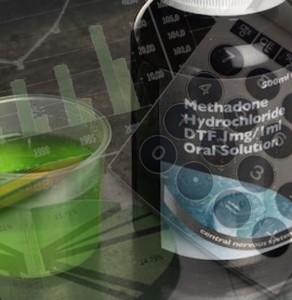
Her suggestion: Apply the same standards to opioid-based treatment that are required of other programs. Focus less on the medication and more on clinical change. At present, the incentive was to get the client on the right dose and drastically reduce the other services. It’s a true medical model, applied to a population with an incredible number of other social and emotional needs, most of which are ignored. “Until somebody can’t pay their bill,” she warned. “When that happens, we’re expected to taper them off the program as soon as we can.”
Economists tell us to look for financial incentives to explain how business models work. In the case of a big methadone program, the incentives are mostly on the side of very long-term maintenance. The medication costs just pennies a day, so most of the program’s expense is in staffing. The fewer services you provide, the fewer staff you need, and the more likely you are to have a healthy profit margin.
Of course, some Opioid Maintenance Therapy (OMT) programs operate on a shoestring, usually because they provide more treatment. Others stick to the minimum and achieve impressive profit margins. It’s a difference in philosophy and approach.
Anyway, that was one person’s experience.










